Prevalence of metabolic syndrome in the clinical practice of general medicine in Italy
Introduction
Metabolic syndrome (MS) is a complex clinical condition, characterized by the concomitant presence in the same individuals of multiple metabolic and cardiovascular (CV) risk factors, including high-normal blood pressure (BP), abdominal obesity, lipid abnormalities [low levels of high-density lipoprotein (HDL) cholesterol and high levels of triglycerides], insulin resistance and impaired fasting glucose tolerance (1). Following this initial definition, other additional features have been proposed to better define patients with MS, among which subclinical pro-inflammatory and pro-thrombotic states have been frequently associated with other metabolic abnormalities observed in these patients (2-5).
Due to its multifactorial pathogenesis and different clinical presentations, the prevalence of MS and its potential impact on global CV risk assessment are still debated (6-10). Particularly, the thresholds for pharmacological and non-pharmacological treatment initiation are quite heterogeneous, thus reflecting not uniform diagnostic and therapeutic approaches by physicians involved in the clinical management of these high risk individuals. In addition, the most recent sets of European guidelines tended to downgrade the clinical relevance of the syndrome (11,12), further contributing to generate misperception of the potential clinical and educational relevance of MS in terms of primary prevention in a setting of real life.
Despite these concerns, in fact, it is out of question the potential clinical impact of this “easy to detect” clinical condition, in order to early intercept and promptly treat those patients at high risk of developing sustained hypertension, diabetes, obesity or atherogenic dyslipidaemia (13). In this view, the presence of MS is associated with a 9-fold increased risk of developing major CV events (14) and mostly a 5-fold increased risk of developing diabetes (15). Thus, educational and therapeutic interventions aimed at properly identifying these high risk individuals may contribute to reduce the burden of CV diseases in the general population (16-18).
On the basis of these considerations, the Osservatorio Regionale sulla Sindrome Metabolica (ORSA) study was designed as a pilot experience to investigate the prevalence of MS in a setting of real practice in Italy. The primary aims of this survey were to evaluate prevalence of MS, and to estimate prevalence of additional CV risk factors and concomitant conditions in patients with MS followed by general practitioners (GPs) in Italy.
Methods
Methodology of the study
The ORSA study is an observational, non-interventional, cross-sectional study designed to evaluate the prevalence of MS and associated CV risk factors among outpatients followed by GPs operating in the setting of real life in Italy.
The study conformed to the Declaration of Helsinki and its subsequent modifications, was approved by the reference Ethical Committee of each participating physician. The confidentiality of the data was carefully and strictly protected. Written consent to participate to the program was obtained by all involved physicians and patients. Confidentiality on demographic and clinical data of individual patients was carefully preserved.
Physicians’ recruitment
Physicians’ recruitment was carried out in 2007. Involved GPs were randomly selected from a community of physicians, who shared some specific features: (I) experience in data collection and clinical case report form (CRF) compilation; (II) a routine practice of at least 60 patients per week, on average; (III) professional expertise in the clinical management of patients with CV and/or metabolic abnormalities. These GPs were distributed in three main areas throughout the Italian territory (Regione Piemonte, Regione Lazio, and Regione Umbria). These areas have been arbitrarily identified from the scientific committee on the basis of the accessibility and clinical experience of the corresponding reference centers (Rome, Turin, Perugia), as well as on the basis of the availability of GPs who have pre-specified professional and clinical skills.
Physicians were invited to participate in a pilot observational study, aimed at evaluating prevalence of MS and associated CV risk factors in their outpatients’ population. Acceptance of this initial invitation placed physicians under no obligation, and physicians were entitled to drop out of the survey at any stage.
Written invitations were forwarded in a sizable number to ensure a sufficient representativity of the study population sample in their own areas, and to achieve this target within a period of approximately 3-4 weeks. Following their acceptance, involved physicians were asked to report clinical data extracted from their clinical records. These data were referred to the first or the last three consecutive adult Caucasian outpatients aged more than 30 years, whatever the reason they referred to their own attending physicians.
The entire data collection was completed by participants on-site and the completed CRFs were then delivered to the Data Collection Centre. Physicians who completed the program did not receive any compensation for their participation.
Data collection
Data collection included medical history and physical examination, anthropometric and clinical parameters, concomitant CV risk factors, current therapy for hypertension, dyslipidaemia, diabetes and other CV diseases, as well as any concomitant medications.
Based on anthropometric data, calculation was made of body mass index (BMI) that was expressed as body weight in kilograms divided by body surface in squared metres. Clinic systolic and diastolic BP levels, serum lipids, blood glucose and glycosylated haemoglobin (Hbc1A) levels were extracted, when available, from available clinical records and generally not exceeding 3 months before observation.
Clinical data were collected into a specific CRF, in which physicians reported presence or absence of different MS criteria, their absolute values and other metabolic and clinical parameters, if available, including CV and metabolic risk factors. With the only exception of anthropometric and BP data, all parameters reported in the CRF were derived from the GPs clinical databases, if available, and were not measured at the time of the observation.
Data analysis
Available data were locally collected and centrally analysed. Normal and abnormal values of different clinic and metabolic parameters were reported in a separate addendum, made available for involved GPs, and indicated as MS criteria in the CRF.
MS was defined according to Adult Treatment Panel (ATP) III definition (19). In particular, the following diagnostic criteria were adopted: BP ≥130/85 mmHg; HDL cholesterol <40 mg/dL in male and <50 mg/dL in female subjects; triglycerides ≥150 mg/dL; fasting glucose ≥110 mg/dL; waist circumference >102 cm in males and >88 cm in females (19).
Statistical analysis
All data were entered into Microsoft Excel for Windows (Microsoft Excel, Microsoft Corp, Redmond, Wash). Continuous variables were expressed as mean ± standard deviation and compared by a Chi-square test. Discrete variables were expressed as percentages and compared by Pearson’s Chi-square test. Because of the relatively small sample size, the comparisons were considered relevant for P<0.05.
Results
Selection of population sample
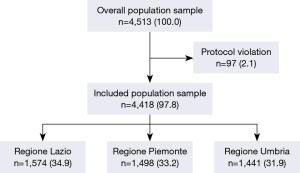
As shown in Figure 1, from an original sample of 4,513 individual outpatients, 95 (2.1%) records were omitted from analysis because of missing or partial clinical data and/or protocol violation (age criterion). Thus, we included an overall population sample of 4,418 outpatients [2,302 females, (mean age, 50.8±11.8 years); BMI, 26.7±4.7 kg/m2), which represents 83.7% of the original population sample was included in the present analysis. This sample was equally distributed into three main areas: 1,574 (34.9%) outpatients from Regione Lazio, 1,498 (33.2%) from Regione Piemonte, and 1,441 (31.9%) from Regione Umbria.
The main reason for medical visit was follow-up of chronic disease (55.5%), followed by acute illness (13.0%), administrative reasons (10.9%), prevention of disease (9.7%), new onset of signs or symptoms (4.5%), and other unspecified reasons (5.3%).
Anthropometric and clinical parameters in the overall population sample
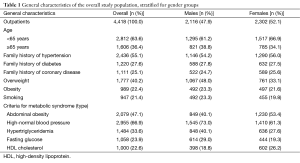
General characteristics of study population are reported in Table 1. No significant difference was found between the two gender groups regarding age, family history of hypertension, diabetes and coronary artery disease, smoking and obesity, though male individuals showed significantly higher prevalence of overweight.
Full table
Metabolic parameters in the overall population sample
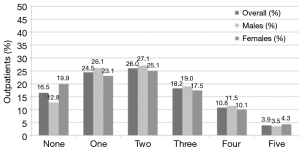
Prevalence of MS is illustrated in Figure 2. MS was found in 1,456 (33.0%) outpatients out of 2,962 (67.0%). In particular, 806 (18.2%) outpatients showed three diagnostic criteria for MS, 476 (10.8%) four criteria and 174 (3.9%) five criteria, without relevant differences between gender groups.
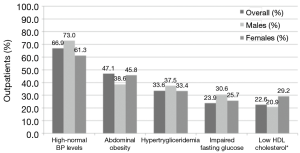
Distribution of different diagnostic criteria for MS is illustrated in Figure 3. High-normal BP was the most common risk factor (n=1,382; 94.9%), followed by abdominal obesity (n=1,229; 84.4%), hypertriglyceridemia (n=1,032; 70.9%), abnormal fasting glucose (n=819; 56.3%) and low HDL cholesterol levels (n=730; 50.1%). Of note, male’s individuals have higher prevalence of high-normal BP levels, hypertriglyceridemia and impaired fasting glucose than female individuals, who have higher prevalence abdominal obesity and lower levels of HDL cholesterol than the former ones.
Anthropometric, clinical and metabolic parameters of outpatients with compared with those without MS are reported in Table 2. Patients with MS were older and more frequently male compared with those without MS. As expected, those outpatients with MS have higher levels of BMI, waist circumference, systolic/diastolic BP levels, triglycerides, fasting glucose, and post-prandial (2 h) glucose than patients without MS. They also showed lower levels of HDL cholesterol, as well as higher levels of total and LDL cholesterol (P<0.001 for all comparisons) than patients without MS.
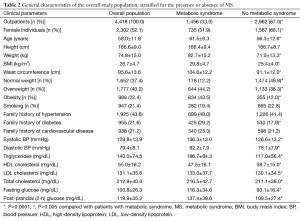
Full table
Among different clinical parameters and various risk factors for MS, male gender, weight-related parameters (waist circumference and presence of obesity), high levels of triglycerides, fasting glucose and systolic BP, as well as low levels of HDL cholesterol were significantly related to an increased risk of having MS (Table 3).
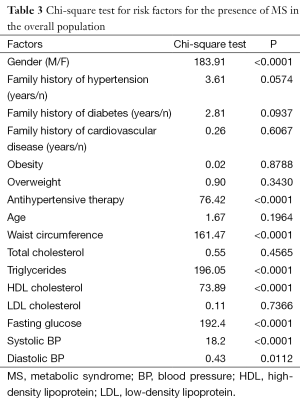
Full table
Clinical and metabolic parameters in outpatients with metabolic syndrome (MS)
No significant differences were found with regard to family history of hypertension, diabetes and coronary artery disease between male and female patients with MS. As observed in the overall population sample, male’s individuals with MS have higher prevalence of high-normal BP levels, hypertriglyceridemia and impaired fasting glucose than female individuals with MS, who have higher prevalence abdominal obesity and lower levels of HDL cholesterol than the former ones.
When available, patients with MS showed normal renal parameters (creatinine, 0.9±0.4 mg/dL and BUN, 28.5±21.3 mg/dL) with relatively low levels of plasma electrolytes (sodium, 105.2±60.7 mEq/L and potassium, 3.4±1.9 mEq/L); in particular, serum uric acid was within normal ranges (4.4±2.7 mg/dL) in MS patients (data not shown).
Associated clinical conditions tended to be more frequently reported in male than in female’s outpatients with MS. In particular, history of coronary artery disease (also including previous myocardial infarction, angina pectoris and coronary revascularization) was more frequently reported in males than in females, as well as cerebrovascular and peripheral artery diseases. Of note, no significant differences were observed in terms of prevalence of diabetes mellitus between two gender groups. Prevalence of renal disease and heart failure was marginal, though higher in male than in female outpatients with MS.
Pharmacological and non-pharmacological treatment
The majority of MS outpatients (n=1,341; 92.1%) received at least one drug for either hypertension, dyslipidaemia or diabetes mellitus. In particular, BP-lowering therapy was the most commonly prescribed pharmacological treatment in this population of adult outpatients with MS, particularly in males than in females (73% vs. 80%, respectively). Among different antihypertensive drug classes, ACE inhibitors were the most frequently used, mostly in males, followed by diuretics (31.3%), angiotensin receptor blockers (25.4%), beta-blockers (21.8%), calcium-channel blockers (19.5%) and other drug classes (4.9%). With the only exception of ARBs and beta-blockers, all the remaining drug classes were more frequently prescribed in male than in female outpatients with MS.
Lipid-lowering therapy was prescribed in about 72% of adult outpatients with MS included in this study. Of note, about 40% were treated with non-pharmacological therapy (e.g. , diet) and about 32% with statins. Lower proportions of patients with MS received a lipid-lowering therapy based on either fibrates (3.7%) or ω-3 (5.2%). While females with MS received more frequently non pharmacological therapy, males with MS were more often treated with lipid-lowering drugs.
Glucose-lowering therapy was prescribed in about 42% of adult outpatients with MS included in this study. In particular, about 19% of outpatients with MS were treated with non-pharmacological therapy (e.g. , diet) whereas about 26% received oral glucose-lowering agents and about 5% received insulin therapy. Males subjects with MS were more frequently treated, both with pharmacological and non-pharmacological treatment, than female’s subjects with MS.
Discussion
The present manuscript reports the main findings of a pilot observational study, aimed at evaluating the prevalence of MS and associated CV risk factors, as well as concomitant clinical conditions in a relatively large population sample of adult outpatients, who were followed in a setting of real life in Italy. The results of this analysis may have relevance for the clinical management of patients with metabolic abnormalities, since they confirmed a relatively high prevalence of MS, suggesting the need for implementing both pharmacological and non-pharmacological interventions in order to reduce the risk of CV and metabolic complications in these high risk individuals. Among the various data made available by this analysis, some specific aspects deserve discussion.
First of all, this study represents the first experience aimed at systematically evaluating the absolute prevalence of MS in adult outpatients from different macro-areas in Italy, reporting that about one third of the patients showed MS. Similar proportion was found in a previous study by Miccoli et al. (20), which adopted the same diagnostic criteria to an adult general population from the area of Lucca. In both studies, MS prevalence progressively increased with ageing, ranging from 3-5% in subjects aged 20-29 years to 25-30% in subjects aged 65-70 years or older. In particular, we found that 34% of female and about 39% of male subjects aged 65 years or older have MS, thus confirming the importance of improving strategies for effective CV risk prevention also in the elderly population (21).
In our sample, only a minority of subjects (16.5%) did not show any relevant metabolic risk factors, having 50% of these patients at least one or two criteria and the remaining 33.5% three or more criteria for the diagnosis of MS. Among these factors, high BP levels represent the most common CV risk factor, followed by abdominal obesity, hypertriglyceridemia, impaired fasting glucose and low HDL cholesterol levels. Similar distribution was also observed in a recent study performed in more than 52,000 hypertensive patients, included in observational studies made available between 2000 and 2005 (22).
In the present analysis, BP levels were within the high-normal ranges, both for the systolic and for the diastolic BP, without relevant differences between two gender groups. Similar findings were also reported in another longitudinal survey, performed in 2006, in which 1,078 physicians collected data of 9,904 outpatients, among which 3,219 (32.5%) were residents in Northern, 3,652 (36.9%) in Central and 3,033 (30.6%) in Southern Regions of Italy (23). Among these patients, hypertension represents the most common CV risk factors, followed by hypercholesterolemia, obesity and diabetes (23). Even in this case, however, prevalence of MS was not assessed.
As observed in previous studies (22,23), the large majority of the outpatients received an antihypertensive drug treatment (80%). In particular, those outpatients with MS have significantly higher levels of systolic/diastolic BP level, despite they received significantly more BP-lowering drugs, than patients without MS, mostly including those drugs able to counteract the abnormal activation of renin-angiotensin system (i.e. , ACE inhibitors and angiotensin receptors blockers).
Observed prevalence of concomitant clinical conditions was also relatively frequent in this population sample. About 58% of the patients had previous CV events and 42% of these patients had at least one previous CV event. Among these, coronary artery disease, including previous myocardial infarction, angina and coronary revascularization, was the most frequent concomitant clinical condition, particularly in male individuals, followed by cerebrovascular, peripheral and renal diseases. Of note, 30% of the patients also had a concomitant diagnosis of diabetes mellitus. All these conditions further increased the risk of developing CV complications, thus highlighting the need for properly identifying patients with MS in a setting of real life, and for adopting effective and well tolerated therapeutic strategies for achieving better CV prevention.
Potential limitations
Some potential limitations should be acknowledged. The present study is based on a cross-sectional, descriptive survey and, as such, it can only identify associations, but it cannot provide insights on causation. In view of the relatively small sample size of our study, even the possibility of sampling bias has to be considered, although proven methods were applied to avoid this. The relatively small sample size and different distribution of involved physicians in three macro-areas may also mean that the views expressed by respondents may not be fully representative of opinions of the wider physician community in our Country. In most cases, dependence on physician self-reporting throughout specifically designed CRF, rather than more direct measures of several clinical parameters, such as lipid or glucose quantifications, which derived from physicians’ own medical databases, may also create potential biases. Our analysis cannot provide information about whether physicians’ practices were located in rural or urban areas. Since access to medical health care in rural areas may be more difficult than in urban areas, this aspect should be acknowledged when considering the higher prevalence of major CV risk factors and associated clinical conditions in Southern than in Northern areas of our country. At the same time, we cannot provide data on the socio-economic position of individual patients. Finally, prognostic value of MS and other metabolic abnormalities in terms of major CV events cannot be evaluated, due to the study design and research protocol.
Conclusions
Using this sample of adult outpatients followed by GPs distributed in three main regions, our analysis reported a relatively high prevalence of MS and high prevalence of associated CV and metabolic risk factors in these high risk individuals compared to those without MS. These findings may have potential impact to better identify those patients with MS at high risk of developing major CV or metabolic complications in a setting of real life in Italy.
Acknowledgements
The authors wish to thank all the involved physicians for their contribution to collect clinical data and the Italian Society of Cardiovascular Prevention (SIPREC) for its endorsement to this educational project. The study was conducted with an unrestricted educational grant from Astra Zeneca.
Footnote
Conflicts of Interest: MV and BT have given lectures at symposia for Astra Zeneca; other authors have no conflicts of interest to declare.
References
- Grundy SM, Cleeman JI, Merz CN, et al. A summary of implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Arterioscler Thromb Vasc Biol 2004;24:1329-30. [PubMed]
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735-52. [PubMed]
- Grassi G, Dell'Oro R, Quarti-Trevano F, et al. Neuroadrenergic and reflex abnormalities in patients with metabolic syndrome. Diabetologia 2005;48:1359-65. [PubMed]
- Cicero AF, Derosa G, Manca M, et al. Vascular remodeling and prothrombotic markers in subjects affected by familial combined hyperlipidemia and/or metabolic syndrome in primary prevention for cardiovascular disease. Endothelium 2007;14:193-8. [PubMed]
- Rubattu S, Sciarretta S, Ciavarella GM, et al. Reduced levels of N-terminal-proatrial natriuretic peptide in hypertensive patients with metabolic syndrome and their relationship with left ventricular mass. J Hypertens 2007;25:833-9. [PubMed]
- Cicero AF, Nascetti S, Noera G, et al. Metabolic syndrome prevalence in Italy. Nutr Metab Cardiovasc Dis 2006;16:e5-6. [PubMed]
- Ambrosioni E, Cicero AF, Parretti D, et al. Global cardiovascular disease risk management in italian patients with metabolic syndrome in the clinical practice setting. High Blood Press Cardiovasc Prev 2008;15:37-45. [PubMed]
- Scholze J, Alegria E, Ferri C, et al. Epidemiological and economic burden of metabolic syndrome and its consequences in patients with hypertension in Germany, Spain and Italy; a prevalence-based model. BMC Public Health 2010;10:529. [PubMed]
- Tocci G, Ferrucci A, Passerini J, et al. Prevalence of 'borderline' values of cardiovascular risk factors in the clinical practice of general medicine in Italy: results of the BORDERLINE study. High Blood Press Cardiovasc Prev 2011;18:43-51. [PubMed]
- Wille E, Scholze J, Alegria E, et al. Modelling the costs of care of hypertension in patients with metabolic syndrome and its consequences, in Germany, Spain and Italy. Eur J Health Econ 2011;12:205-18. [PubMed]
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159-219. [PubMed]
- Authors/Task Force Members. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013;34:3035-87. [PubMed]
- Sesti G, Volpe M, Cosentino F, et al. Metabolic Syndrome: Diagnosis and Clinical Management, an Official Document of the Working Group of the Italian Society of Cardiovascular Prevention (SIPREC). Guest Editor: E. Agabiti Rosei, President of the Italian Society of Hypertension. High Blood Pressure & Cardiovascular Prevention 2006;13:185-98.
- Volpe M, Battistoni A, Tocci G, et al. Cardiovascular risk assessment beyond Systemic Coronary Risk Estimation: a role for organ damage markers. J Hypertens 2012;30:1056-64. [PubMed]
- Sattar N, Gaw A, Scherbakova O, et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 2003;108:414-9. [PubMed]
- Cicero AF, Derosa G, Bove M, et al. Effect of a sequential training programme on inflammatory, prothrombotic and vascular remodelling biomarkers in hypertensive overweight patients with or without metabolic syndrome. Eur J Cardiovasc Prev Rehabil 2009;16:698-704. [PubMed]
- Wagner A, Dallongeville J, Haas B, et al. Sedentary behaviour, physical activity and dietary patterns are independently associated with the metabolic syndrome. Diabetes Metab 2012;38:428-35. [PubMed]
- Cicero AF, Tartagni E, Ertek S. Nutraceuticals for metabolic syndrome management: from laboratory to benchside. Curr Vasc Pharmacol 2014;12:565-71. [PubMed]
- Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Arterioscler Thromb Vasc Biol 2004;24:e149-61. [PubMed]
- Miccoli R, Bianchi C, Odoguardi L, et al. Prevalence of the metabolic syndrome among Italian adults according to ATP III definition. Nutr Metab Cardiovasc Dis 2005;15:250-4. [PubMed]
- Vishram JK, Borglykke A, Andreasen AH, et al. Impact of age and gender on the prevalence and prognostic importance of the metabolic syndrome and its components in Europeans. The MORGAM Prospective Cohort Project. PLoS One 2014;9:e107294. [PubMed]
- Volpe M, Tocci G, Trimarco B, et al. Blood pressure control in Italy: results of recent surveys on hypertension. J Hypertens 2007;25:1491-8. [PubMed]
- Tocci G, Ferrucci A, Guida P, et al. Global cardiovascular risk management in different Italian regions: an analysis of the Evaluation of Final Feasible Effect of Control Training and Ultra Sensitisation (EFFECTUS) educational program. Nutr Metab Cardiovasc Dis 2012;22:635-42. [PubMed]