Appropriateness and diagnostic yield of cardiac magnetic resonance imaging from a tertiary referral center in the Middle East
Introduction
Cardiac magnetic resonance imaging (CMRI) is a novel non-invasive imaging modality that was introduced in clinical practice since the 1990’s. It provides high quality images with pertinent information on anatomy, tissue characterization, function, hemodynamics, and others (1). Its clinical applications have expanded over time and include detection of coronary artery disease (2-4), viability and scar burden (5), differentiating types of cardiomyopathy (6-10), assessment of cardiac masses and vascular structures (11). It also provides the tools for risk stratification and guiding therapy (12,13).
In order to standardize the utilization of this modality and avoid unnecessary testing, and under the auspices of the American College of Cardiology Foundation (ACCF), together with key specialty and subspecialty societies (including Society of CMR), that the 2006 appropriateness criteria were developed (14). They were then adopted and updated by the Asian Society of Cardiac Imaging in 2010 (15). The technique however, was only recently introduced in the Middle East and is not readily available except at few academic tertiary centers. In Lebanon, a comprehensive CMR program was launched on January 1st 2013 at our institution. The test is relatively (16) expensive and often represents a financial challenge to patients and third party payers, particularly with such economic constraint in the society. Hence, we sought to assess the appropriateness of CMR testing at our institution since its inception and over the first year and a half; and to evaluate the clinical yield of the studies in order to optimize future performance, provide standard of care testing in compliance with the guidelines, and avoid unnecessary testing.
Methods
Patient selection
All patients that underwent clinical CMR between January 1st 2013 [starting date of the launch of the comprehensive CMR program at the American University of Beirut Medical Center (AUBMC)] and June 18th 2014 were included in the study. None of the patients were excluded. Patients’ demographics (age, gender, body mass index), referral pattern, specialty of the referring physicians, indication, clinical findings including the presence of incidentals were retrospectively extracted from the report. The study was approved by the Institutional Review Board at AUBMC.
Cardiac magnetic resonance imaging (CMRI)
CMR studies were performed on Philips Ingenia 3.0 T and 1.5 T release 4.1.1 (Eindhoven, Netherlands) scanners. The latter was reserved for patients with suspicion of cardiac siderosis. Prior to the imaging, a cardiologist (Wael AlJaroudi, Hussain Isma’eel) reviewed the request, clinical indication and patient history, in order to set up the appropriate CMR protocol, but without excluding any request (hence minimizing selection bias). Turbo spin echo and gradient echo images were obtained for anatomic definition, while dynamic cine images [balanced fast field echo (B-FFE)] for the evaluation of cardiac function and valvular analysis. Phase contrast was used to assess hemodynamics, calculate flow and shunt fraction. On selected patients and depending on the indication, contrast enhanced volumes sets were acquired for 3-D MRA (magnetic resonance angiogram) reconstructions after use of gadolinium dotaram (0.5 mmol/mL, 0.1 mmol/kg) with advanced off-line 3-D post-processing using multiplanar reconstructions for optimal morphologic evaluation. Delayed gadolinium-enhancement (phase sensitive inversion recovery) analysis was performed to assess for viability, scar volume quantification (using standard semi-automated method) and infiltrative disease. Finally, for patients with clinical suspicion of iron overload, T2* imaging (turbo fast echo with multiple echoes) was performed to assess for iron content in the heart and liver.
Appropriateness
All CMR reports were retrieved and retrospectively reviewed by a level III CMR trained and certified physician (Wael AlJaroudi). The clinical history, indication of the CMR study and findings were extracted from the CMR report. The indications were coded according to the 2010 updated Asian Society of Cardiac Imaging guidelines with their corresponding appropriateness level {A [7-9]: appropriate; U [4-6]: uncertain; I [1-3]: inappropriate} (Table 1) (15). Given the close similarity of these guidelines to the 2006 multi-society appropriateness criteria (14), coding and analyzing the data using the other guidelines yielded same appropriate utilization rate.
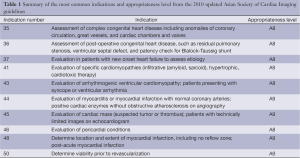
Full table
Diagnostic yield
The usefulness of the CMR study was judged on whether if fulfilled any of the following pre-specified criteria: (I) provided relevant findings that were missed or could not be detected on transthoracic echocardiogram; (II) confirmed a clinical diagnosis that was suspected on other imaging modality; (III) corrected a diagnosis that was falsely made prior to the CMR; (IV) provided accurate evaluation and quantification that have impact on guiding therapy; (V) provided information on scar burden for risk factor stratification; (VI) ruled out infiltrative cardiomyopathy; or (VII) was not helpful and did not add any relevant information. Incidental extra-cardiac findings were also documented and extracted for analysis.
Statistical analysis
Continuous data were expressed as a mean ± one standard deviation or median (25th and 75th percentile), while categorical data were displayed as frequencies and percentage. Pie and bar diagrams were used for figure illustration. All statistical analyses were performed using the Statistical Package for Social Sciences, version 19, for Windows (SPSS, Chicago, Illinois, USA).
Results
Patient characteristics
A total of 142 patients [mean age 42.1 (SD: 18) years, 24.6% females] underwent CMR between January 1st 2013 and June 18th 2014 (Table 2).
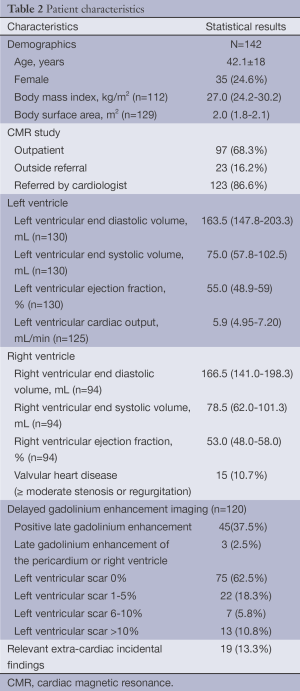
Full table
Pattern of referral
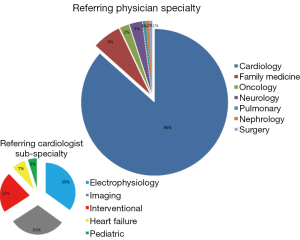
Almost two-thirds of studies were performed on an outpatient basis. Referrals from within the institution constituted the majority of cases (83.8%), with 16.2% of the studies being referred from other hospitals and private practices. The specialty and sub-specialty of the referring physicians are illustrated in Figure 1. The cardiologists referred 122 cases (86%) with main contribution from electrophysiology and imaging specialists, followed by the interventional and heart failure.
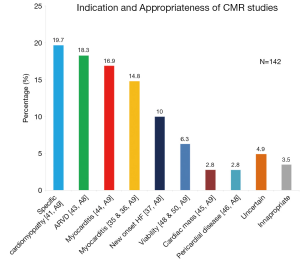
Appropriateness of CMR studies
The indications of the CMR studies are summarized in Figure 2. The most common ones included assessment of specific cardiomyopathies (infiltrative, amyloid, sarcoid, hypertrophic, post-cardiotoxic therapy), arrhythmogenic right ventricular dysplasia, myocarditis, and congenital cases. CMR studies to assess for new onset heart failure etiology, viability, cardiac masses and pericardial diseases constituted the remaining 21.9% of the studies. The appropriateness level for each of the indication is listed in Figure 2 (A8-A9). There were an additional of 12 cases (8.4%) that were referred for seemingly appropriate indications; however, on careful review of the clinical history, they were deemed as uncertain or inappropriate. The details of these 12 cases are summarized in Table 3. The appropriate utilization rate was similar when using the 2006 multi-society guidelines (14).
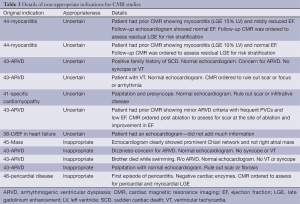
Full table
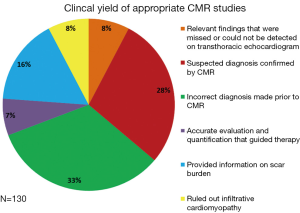
Diagnostic yield
Of the 142 CMR studies, 12 were considered to have uncertain or inappropriate indications, and none of them provided any additional information beyond the echocardiogram or clinical history. Of the remaining 130 appropriate cases, the diagnostic yield of the studies is summarized in Figure 3. Almost one-third of cases had an incorrect diagnosis prior to CMR. An additional of 8% of cases had relevant findings that were missed on other studies (example anomalous pulmonary veins, sinus venosus defect, etc.). In addition, CMR helped confirm the diagnosis in 28% of cases, and provided accurate quantification to guide optimal therapy (for example, quantification of pulmonary regurgitation fraction and right ventricular end-diastolic volume index to guide optimal timing of pulmonary valve replacement in patients with tetralogy of Fallot; shunt fraction; quantification of ejection fraction to decide on implantable cardiac defibrillator) (Figure 4).
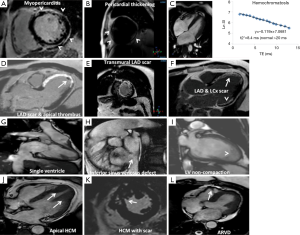
Late gadolinium enhancement
A total of 120 patients (84.5%) underwent delayed gadolinium enhancement imaging. More than one-third of patients (n=45, 37.5%) had evidence of late-gadolinium enhancement. The distribution of scar volume quantification of the total LV included 18.3% with scar 1-5%, 5.8% with scar 6-10%, and 10.8% with scar >10% (Table 1). There were 9/45 patients (20%) that had scar in an ischemic distribution, one patient with scar in both ischemic and non-ischemic pattern, and with the remaining patients (78%) having scar in non-coronary artery disease territory.
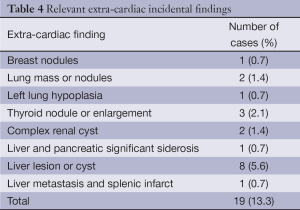
Extra-cardiac incidental findings
A total of 19 (13.3%) extra-cardiac findings were identified and summarized in Table 4. One of the incidental findings (liver metastasis and splenic infarct) was previously known to the reader and prior identified on an abdominal computed tomography study, while the remaining 18 findings were not previously known.
Full table
Discussion
Cardiovascular imaging is a mainstay of contemporary practice, and plays a valuable role in the clinical management and guiding therapy of patients. The rapid evolution of technology with enhanced clinical application has promoted the growth of cardiac imaging. CMR for example provides several advantages to echocardiography particularly when there is a clinical need to assess and quantify the presence of scar, differentiate types of cardiomyopathy, RV quantification, provide tissue characterization, anatomic definition when echocardiography is limited by poor acoustic window, complex congenital cases with 3D volume reconstruction, and several others. However, there has been a parallel growth and fear of over-utilization, inappropriate testing, and the subsequent cost burden on third-party payers, patients and society. Hence, through the development of guidelines and appropriateness criteria, physicians have directed their efforts to eliminate unnecessary testing, and promote cost-conscious utilization of imaging and resources (17).
In the current retrospective analysis of all CMR studies performed at our institution since the inception of the program, 8.4% of the studies were not appropriate and did not yield relevant clinical information beyond what was known or suspected. Of the appropriate studies, CMR changed the diagnosis in one-third of cases, detected new pathology in 8% of cases, and showed important extra-cardiac findings in 9% of studies. One of the main strength of the paper is that it shows that one-third had an incorrect diagnosis prior to CMR. This is perhaps not unique to the Middle East or our institution, and had there been more cases, then many more patients would have benefited from this important technology. This brings out the issue of underutilization. This technology that has been present since 1990’s has only started making its way in Lebanon.
This is the first study to our knowledge that evaluates appropriate CMR testing in accordance to recently published and revised guidelines. There have been several studies assessing appropriateness of other non-invasive testing in the region. For cardiac computed tomography (CCT), for example, El Sibai et al. showed improvement in the appropriate utilization of CCT from 8% in 2006 to 38% in 2010 at the same institution in Lebanon (18). In addition, Gholamrezanezhad et al. showed a 72.5% appropriate utilization of single photon emission computed tomography myocardial perfusion imaging in Iran in 2011 (19). Similarly, Gibbons et al. showed a 64% appropriate indication for stress nuclear imaging and stress echocardiography in the United States in 2008 (20). Gibbons et al. showed that adopting the guidelines results in improvement of appropriate testing with time (21).
The relatively high appropriate utilization of CMR studies at our institution is likely related to several factors. First, the referring physician most often contacted one of the imaging cardiologists or radiologists to discuss the case and the question in mind that the CMR study is supposed to answer before sending the patient for the study. In the era of multimodality imaging, identifying which modality is the best to answer the question posed is recognized as part of the guidance duties of the cardiovascular imaging specialists (17). This is in the best interest of the patient to reduce unnecessary testing and hazardous exposures. Furthermore, given the worldwide observed increase in the cost incurred by the healthcare system to imaging in general, such practice, and not an unhealthy inter-modality specialists’ competition, is foreseen as the best way to address cost increase concerns (17).
Second, as part of maintaining quality assurance, both cardiologists (Wael AlJaroudi and Hussain Isma’eel) randomly reviewed every other month few cases that were performed and interpreted by the other physician for appropriate indications and result interpretations. While this may not have impacted directly the results of this manuscript (given that all requests were performed and analyzed), it might have had a future impact on subsequent ordered studies and perhaps indirectly biased or discourage us against ordering such un-indicated studies. In the Middle East, assessment of appropriate indication as a quality metric is not widely practiced nor properly publicized, with certain factors leading to unwillingness to report (22). The healthcare administrative environment is not at a similar stage as their counterparts in the USA and Europe (23,24). Some insurance companies, however, do have a pre-approval requirement for certain studies, as is the case with CMR. These impose stringent criteria for approval, something not practiced with echocardiography, probably because CMR is being newly introduced and is more costly. However, even within the more affluent Gulf states in the region, healthcare cost constitutes a significant proportion of the national gross domestic product and is on the rise (Data from the World Bank: http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS), and therefore appropriate utilization assessment is bound to become more widely implemented soon.
Third, the CMR appropriateness criteria have been available and well known since 2006 and as the authors have experience in CMR for many years as part of their training abroad, this could have contributed to the high appropriate utilization rate. This in turn highlights the advantages of having healthcare professional societies (Society of CMR, Society of CCT, European Society of Cardiology, European Association of Cardiovascular Imaging, American Heart Association, American College of Cardiology, and others) being at the forefront of setting appropriateness criteria before insurance companies and government do that for us; and suggests that an earlier formal introduction of these concepts into the training of physicians might be useful in a changing healthcare environment.
Limitations
We recognize several limitations of the study. First, this is a retrospective study from a single tertiary referral center. We analyzed all patients including the first one since the initiation of the CMR program to minimize any potential selection bias. In addition, the evaluation of coronary artery disease and ischemia using stress testing CMR is not yet available at our institution. Hence, there were several potential appropriateness indications for the detection coronary artery disease, risk stratification, and preoperative evaluation that could not be evaluated, and therefore skewed our results. In the next few months, we will be launching stress CMR and we should be able to evaluate the appropriateness of these studies in the coming few years. Furthermore, we did not have any follow-up data to document impact on clinical management or outcome. We are currently preparing to build a prospective database with follow-up data. Finally, most of the referrals were internal and from cardiologists. Still, this manuscript represents one of the first experiences of a tertiary center in Lebanon and the region, and reflects an unbiased view of our population.
Future directions
With the expansion of the CMR program and introduction of stress CMR, cardio-oncology and hematology program, and adult congenital heart disease, we expect a steady increase in volume and widening of the types of studies and indications. It is imperative to continue to perform appropriate CMR studies when indicated, and minimize unnecessary tests particularly given the cost and financial burden on the society. Furthermore, it is important to build a prospective database with clinical follow-up, which is work in progress.
Conclusions
Despite the recent launch of the CMR program at our institution, the majority of studies were appropriately indicated, provided relevant data and were clinically useful. Inappropriate or uncertain studies did not provide relevant data beyond what was known or expected, and should be minimized to avoid unnecessary costs. Large prospective CMR database with clinical follow-up is needed to provide more insight about cardiovascular disease and outcomes in our population.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Kramer CM, Barkhausen J, Flamm SD, et al. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson 2013;15:91. [PubMed]
- Jogiya R, Kozerke S, Morton G, et al. Validation of dynamic 3-dimensional whole heart magnetic resonance myocardial perfusion imaging against fractional flow reserve for the detection of significant coronary artery disease. J Am Coll Cardiol 2012;60:756-65. [PubMed]
- Manka R, Paetsch I, Kozerke S, et al. Whole-heart dynamic three-dimensional magnetic resonance perfusion imaging for the detection of coronary artery disease defined by fractional flow reserve: determination of volumetric myocardial ischaemic burden and coronary lesion location. Eur Heart J 2012;33:2016-24. [PubMed]
- Hamon M, Fau G, Née G, et al. Meta-analysis of the diagnostic performance of stress perfusion cardiovascular magnetic resonance for detection of coronary artery disease. J Cardiovasc Magn Reson 2010;12:29. [PubMed]
- Rajiah P, Desai MY, Kwon D, et al. MR imaging of myocardial infarction. Radiographics 2013;33:1383-412. [PubMed]
- Patel MR, Cawley PJ, Heitner JF, et al. Detection of myocardial damage in patients with sarcoidosis. Circulation 2009;120:1969-77. [PubMed]
- Karamitsos TD, Francis JM, Myerson S, et al. The role of cardiovascular magnetic resonance imaging in heart failure. J Am Coll Cardiol 2009;54:1407-24. [PubMed]
- Thavendiranathan P, Wintersperger BJ, Flamm SD, et al. Cardiac MRI in the assessment of cardiac injury and toxicity from cancer chemotherapy: a systematic review. Circ Cardiovasc Imaging 2013;6:1080-91. [PubMed]
- Leong DP, De Pasquale CG, Selvanayagam JB. Heart failure with normal ejection fraction: the complementary roles of echocardiography and CMR imaging. JACC Cardiovasc Imaging 2010;3:409-20. [PubMed]
- White JA, Kim HW, Shah D, et al. CMR imaging with rapid visual T1 assessment predicts mortality in patients suspected of cardiac amyloidosis. JACC Cardiovasc Imaging 2014;7:143-56. [PubMed]
- Fussen S, De Boeck BW, Zellweger MJ, et al. Cardiovascular magnetic resonance imaging for diagnosis and clinical management of suspected cardiac masses and tumours. Eur Heart J 2011;32:1551-60. [PubMed]
- Aljaroudi WA, Flamm SD, Saliba W, et al. Role of CMR imaging in risk stratification for sudden cardiac death. JACC Cardiovasc Imaging 2013;6:392-406. [PubMed]
- Leyva F, Foley PW. Current and future role of cardiovascular magnetic resonance in cardiac resynchronization therapy. Heart Fail Rev 2011;16:251-62. [PubMed]
- Hendel RC, Patel MR, Kramer CM, et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol 2006;48:1475-97. [PubMed]
- ASCI CCT and CMR Guideline Working Group, Kitagawa K, Choi BW, et al. ASCI 2010 appropriateness criteria for cardiac magnetic resonance imaging: a report of the Asian Society of Cardiovascular Imaging cardiac computed tomography and cardiac magnetic resonance imaging guideline working group. Int J Cardiovasc Imaging 2010;26:173-86. [PubMed]
- Long-term results of prospective randomised study of coronary artery bypass surgery in stable angina pectoris. European Coronary Surgery Study Group. Lancet 1982;2:1173-80. [PubMed]
- Hendel RC. Utilization management of cardiovascular imaging pre-certification and appropriateness. JACC Cardiovasc Imaging 2008;1:241-8. [PubMed]
- El Sibai K, Itani S, Rabah A, et al. Evaluation of the appropriateness criteria for coronary computed tomography angiography in an academic medical center in a developing country: comparison of the 2006 and 2010 criteria. J Nucl Cardiol 2011;18:1053-8. [PubMed]
- Gholamrezanezhad A, Shirafkan A, Mirpour S, et al. Appropriateness of referrals for single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) in a developing community: a comparison between 2005 and 2009 versions of ACCF/ASNC appropriateness criteria. J Nucl Cardiol 2011;18:1044-52. [PubMed]
- Gibbons RJ, Miller TD, Hodge D, et al. Application of appropriateness criteria to stress single-photon emission computed tomography sestamibi studies and stress echocardiograms in an academic medical center. J Am Coll Cardiol 2008;51:1283-9. [PubMed]
- Gibbons RJ, Askew JW, Hodge D, et al. Temporal trends in compliance with appropriateness criteria for stress single-photon emission computed tomography sestamibi studies in an academic medical center. Am Heart J 2010;159:484-9. [PubMed]
- Saleh SS, Alameddine MS, Natafgi NM. Acceptability of quality reporting and pay for performance among primary health centers in Lebanon. Int J Health Serv 2013;43:761-77. [PubMed]
- El-Jardali F, Lavis JN, Ataya N, et al. Use of health systems evidence by policymakers in eastern Mediterranean countries: views, practices, and contextual influences. BMC Health Serv Res 2012;12:200. [PubMed]
- Saleh SS, Alameddine MS, Natafgi NM, et al. The path towards universal health coverage in the Arab uprising countries Tunisia, Egypt, Libya, and Yemen. Lancet 2014;383:368-81. [PubMed]


