Evidence for myocardial CT perfusion imaging in the diagnosis of hemodynamically significant coronary artery disease
Coronary computer tomography angiography (CCTA) is a well-established imaging modality in the diagnosis of coronary artery disease (CAD) due to its less invasiveness, high diagnostic value, and widespread availability (1,2). With rapid technological improvements in multislice CT scanners, CCTA has superior spatial resolution enabling it to offer excellent visualization of anatomical details of coronary arteries which allows for a comprehensive assessment of coronary plaques in terms of plaque components (3-5). However, CCTA has limited value in the diagnostic evaluation of myocardial ischemia. The presence of anatomic stenosis does not necessarily relate to functional significance of CAD, which refers to decreased myocardial perfusion (6). Studies have shown that CCTA has limited diagnostic value for assessment of abnormal myocardial perfusion in patients with more than 50% coronary stenosis when compared to myocardial perfusion imaging, single photon emission CT (SPECT) (7,8). Although cardiac positron emission tomography (PET) is superior to SEPCT in the assessment of myocardial ischemia, it is not widely available as opposed to SPECT (9). Furthermore, the high cost of PET camera and cyclotron technology limit the extensive use of this technique in many clinical centers. Currently, SPECT has been well established as the first line diagnostic test for the diagnostic evaluation of patients with CAD as current research evidence is limited with regard to using CCTA as the first line test (Figures 1,2) (6,10).
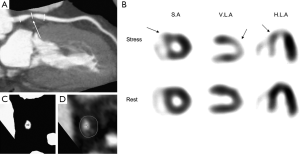
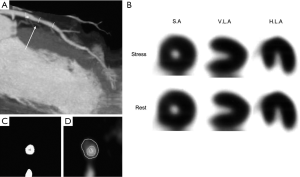
Diagnostic performance of SPECT in myocardial perfusion imaging is limited by low spatial resolution and may miss small or subendocardial areas of hypoperfusion. In addition, attenuation artifact is a well-recognized factor that limits the diagnostic value of SPECT for the detection of myocardial perfusion defects (11). Myocardial CT perfusion imaging has been recently introduced into clinical practice with promising results reported. Studies based on single center experiences have shown that myocardial CT perfusion imaging has moderate to high diagnostic accuracy in the identification of hemodynamically significant coronary stenosis (12). Moreover, a combination of CCTA and myocardial CT perfusion has been shown to improve the diagnostic value of myocardial CT perfusion imaging for accurate detection of myocardial ischemia (13,14). Despite promising reports available in the literature, there is a lack of sufficient data on the clinical outcome of CT perfusion imaging. In contrast, a wealth of data is available indicating the independent prognostic value of myocardial perfusion SPECT imaging in predicting clinical outcomes such as development of cardiac event rate (15). Furthermore, multicenter studies with inclusion of a large cohort of population are necessary to further validate the diagnostic performance of myocardial CT perfusion imaging compared to the reference standard SPECT.
In the 2014 August issue of the Radiology, George et al. conducted a secondary analysis of the CORE320 study by comparing myocardial CT perfusion imaging with SPECT perfusion in the diagnostic assessment of significant coronary stenosis with invasive coronary angiography as the reference method (16). This is a prospective, multicentre study consisting of 381 patients which were recruited at 16 centers at eight countries. All patients underwent resting CCTA and an adenosine stress myocardial CT perfusion imaging, as well as either an exercise or pharmacologic SPECT myocardial perfusion imaging. CCTA data were not included in the analysis as this study mainly focused on the CT perfusion imaging. A 13-segment myocardial model was used to analyse rest and stress myocardial segments with summed stress score (SSS) being calculated as the sum of all segmental scores based on myocardial CT perfusion and SPECT imaging modalities. On per-patient and per-vessel analysis, the sensitivity of CT perfusion imaging were 88% and 78%, which are significantly higher than those of SPECT, which were 62% and 54% (P<0.05), respectively. In contrast, the specificity of SPECT imaging was 67% and 81% at per-patient and vessel analysis, which is significantly higher than that of CT perfusion imaging, which was 55% and 62% (P<0.05), respectively. The area under the receiver operating characteristic curve (AUC) for CT perfusion imaging at per-patient and per-vessel analysis was 0.78 and 0.74, which is significantly higher than that for SPECT imaging, which was 0.69 and 0.69 (P<0.05), respectively. Furthermore, CT perfusion imaging demonstrates significantly higher sensitivity than that of SPECT imaging for assessment of left main, three-vessel, two-vessel and one-vessel disease.
There are three observations from George’s study that bear discussion. First, high sensitivity has been achieved for CT perfusion imaging of hemodynamically significant coronary stenosis when compared to SPECT perfusion imaging in these patients with high prevalence of CAD (60%). This is consistent with reports in the literature. Most of the studies evaluating myocardial CT perfusion imaging are conducted using 64-detector row CT and have shown diagnostic accuracy comparable to SPECT perfusion imaging (17). Recently, high diagnostic accuracy of CT perfusion imaging has been reported in studies using 320-slice CT (18,19). George et al. compared CT perfusion imaging with CCTA and SPECT in 50 symptomatic patients suspected of CAD with SPECT as the reference standard to determine reversible ischemia. CT perfusion imaging shows better performance than CCTA in predicting myocardial ischemia, with sensitivity and specificity of 72% and 91%, with an AUC of 0.81. Excellent performance was found in the detection of myocardial ischemia in the presence of ≥50% stenosis on CCTA (CT perfusion imaging vs. CCTA + SPECT), with sensitivity and specificity of 100%, and 81%, with an AUC of 0.92 (18). With CCTA added to the myocardial CT perfusion imaging, the combined methods have been reported to improve diagnostic value of myocardial CT perfusion imaging, according to an early report by Nasis et al. and the most recent CORE320 study (14,19).
Second, the low specificity of myocardial CT perfusion imaging might be due to inclusion of the high risk population in this study, as 67% patients had intermediate and 31% had high risk of CAD, with the mean calcium score of 423. It is well known that the specificity of CCTA is limited in patients with high calcium scores (>400) due to blooming artifacts which result in overestimation of coronary lesion stenosis, leading to high false positive findings (20). In George’s study, the specificity of CT perfusion imaging on per-patient analysis was 55%, and on per-vessel (all vessels) and individual left anterior descending, left circumflex and right coronary artery analysis, the specificity was 62%, 55%, 56% and 75%, respectively, which is much lower than that reported in other studies (>75% in most of the reports) (12). Although authors addressed in their study limitations that the reason of false positive findings in myocardial CT perfusion imaging might be due to beam-hardening artifacts, they did not analyse plaque composition in relation to the diagnostic value of CT perfusion imaging. Thus, further studies with analysis of coronary plaque component could help to clarify reasons contributing to the low specificity, in particular, differentiation of calcified from non-calcified plaques and corresponding diagnostic value of CT perfusion imaging.
Third, attenuation correction was not used in SPECT imaging, which contributes to the low diagnostic value of SPECT imaging to some extent. Specifically, CT information-based data facilitate attenuation correction and localization that improves both the contrast and diagnostic accuracy of myocardial perfusion imaging performed with SPECT (21). CT-based attenuation correction has been shown to improve diagnostic accuracy, in particular the specificity (22,23). Although the specificity of SPECT imaging is higher than that of CT perfusion imaging as reported in George’s study, with 67% on per-patient analysis, and 74-86% on per-vessel analysis, it is lower than that reported in the literature. In better designed studies, the specificity of myocardial perfusion SPECT imaging is within the range of 85-90% (15). Therefore, use of attenuation correction in SPECT imaging could further enhance the diagnostic value, especially the specificity in the detection of hemodynamically significant CAD.
In summary, this multicenter study has shown high diagnostic sensitivity of myocardial CT perfusion imaging when compared to SPECT for the diagnosis of significant coronary stenosis (>50%) on per-patient and per-vessel analysis. Despite the prospectively designed study conducted at 16 centers, the limited specificity of CT perfusion imaging could be due to blooming artifacts resulting from inclusion of high risk patients, particularly those with high calcium scores. The moderate specificity of SPECT in this study might be caused by lack of use of attenuation correction in SPECT imaging. Using an anatomic marker of >50% stenosis as the reference method is another limitation for assessing myocardial perfusion imaging as invasive angiography is the gold standard for the diagnosis of obstructive coronary stenosis, but it does not predict myocardial ischemia. Invasive fractional flow reserve (FFR) is a lesion-specific technique that is widely used as the gold standard physiologic test for assessment of functional significance of a coronary lesion (24,25). Further studies are needed to address these factors that affect the diagnostic performance of both myocardial CT perfusion and SPECT imaging.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Sun Z, Cao Y, Li HF. Multislice computed tomography angiography in the diagnosis of coronary artery disease. J Geriatr Cardiol 2011;8:104-13. [PubMed]
- Sun Z, Choo GH, Ng KH. Coronary CT angiography: current status and continuing challenges. Br J Radiol 2012;85:495-510. [PubMed]
- Sun Z, Xu L. Coronary CT angiography in the quantitative assessment of coronary plaques. Biomed Res Int 2014;2014:346-80.
- Voros S, Rinehart S, Qian Z, et al. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging 2011;4:537-48. [PubMed]
- Fischer C, Hulten E, Belur P, et al. Coronary CT angiography versus intravascular ultrasound for estimation of coronary stenosis and atherosclerotic plaque burden: a meta-analysis. J Cardiovasc Comput Tomogr 2013;7:256-66. [PubMed]
- Sato A, Hiroe M, Tamura M, et al. Quantitative measures of coronary stenosis severity by 64-Slice CT angiography and relation to physiologic significance of perfusion in nonobese patients: comparison with stress myocardial perfusion imaging. J Nucl Med 2008;49:564-72. [PubMed]
- Hachamovitch R, Di Carli MF. Nuclear cardiology will remain the "gatekeeper" over CT angiography. J Nucl Cardiol 2007;14:634-44. [PubMed]
- Tamarappoo BK, Gutstein A, Cheng VY, et al. Assessment of the relationship between stenosis severity and distribution of coronary artery stenoses on multislice computed tomographic angiography and myocardial ischemia detected by single photon emission computed tomography. J Nucl Cardiol 2010;17:791-802. [PubMed]
- Al Moudi M, Sun ZH. Diagnostic value of (18)F-FDG PET in the assessment of myocardial viability in coronary artery disease: A comparative study with (99m)Tc SPECT and echocardiography. J Geriatr Cardiol 2014;11:229-36. [PubMed]
- Trzaska ZJ, Cohen MC. SPECT vs CT: CT is not the first line test for the diagnosis and prognosis of stable coronary artery disease. J Nucl Cardiol 2013;20:473-8. [PubMed]
- Dvorak RA, Brown RK, Corbett JR. Interpretation of SPECT/CT myocardial perfusion images: common artifacts and quality control techniques. Radiographics 2011;31:2041-57. [PubMed]
- Xu L, Sun Z, Fan Z. Noninvasive Physiologic Assessment of Coronary Stenoses Using Cardiac CT. Biomed Res Int 2014;2015:435737-48.
- Rochitte CE, George RT, Chen MY, et al. Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J 2014;35:1120-30. [PubMed]
- Feuchtner G, Goetti R, Plass A, et al. Adenosine stress high-pitch 128-slice dual-source myocardial computed tomography perfusion for imaging of reversible myocardial ischemia: comparison with magnetic resonance imaging. Circ Cardiovasc Imaging 2011;4:540-9. [PubMed]
- Sun Z, Azizi A, Yusof AK. Cardiac nuclear imaging: current status and future directions. Curr Med Imaging Rev 2013;9:170-83.
- George RT, Mehra VC, Chen MY, et al. Myocardial CT perfusion imaging and SPECT for the diagnosis of coronary artery disease: a head-to-head comparison from the CORE320 multicenter diagnostic performance study. Radiology 2014;272:407-16. [PubMed]
- Becker A, Becker C. CT imaging of myocardial perfusion: possibilities and perspectives. J Nucl Cardiol 2013;20:289-96. [PubMed]
- George RT, Arbab-Zadeh A, Miller JM, et al. Computed tomography myocardial perfusion imaging with 320-row detector computed tomography accurately detects myocardial ischemia in patients with obstructive coronary artery disease. Circ Cardiovasc Imaging 2012;5:333-40. [PubMed]
- Nasis A, Ko BS, Leung MC, et al. Diagnostic accuracy of combined coronary angiography and adenosine stress myocardial perfusion imaging using 320-detector computed tomography: pilot study. Eur Radiol 2013;23:1812-21. [PubMed]
- Sun Z, Ng CK. High calcium scores in coronary CT angiography: effects of image post-processing on visualization and measurement of coronary lumen diameter. J Med Imaging Health Inf 2015;5:110-6.
- Sun Z, Muhamad M. AbAziz A. Dosimetry of CT-based attenuation correction for single photon emission computed tomography/computed tomography examinations. J Med Imaging Health Inf 2014;4:743-8.
- Links JM, DePuey EG, Taillefer R, et al. Attenuation correction and gating synergistically improve the diagnostic accuracy of myocardial perfusion SPECT. J Nucl Cardiol 2002;9:183-7. [PubMed]
- Shotwell M, Singh BM, Fortman C, et al. Improved coronary disease detection with quantitative attenuation-corrected Tl-201 images. J Nucl Cardiol 2002;9:52-62. [PubMed]
- Fearon WF, Bornschein B, Tonino PA, et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 2010;122:2545-50. [PubMed]
- De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991-1001. [PubMed]


