Correlates of objectively measured physical activity in cardiac patients
Introduction
Worldwide, coronary heart disease (CHD) is the leading cause of death, accounting for over 13% of all death in middle-to-high-income countries, and its prevalence continues to increase (1). There are currently over 26 million non-institutionalized cardiac patients in the U.S., and survival of those patients need to be improved via cost-effective interventions (2), such as cardiac rehabilitation programs (CRP). CRP centered on regular exercise programming has been shown to be effective in improving cardiovascular health in cardiac patients (3,4). However, despite the well-known benefits of regular physical activity (PA) on long-term health (5-7), many cardiac patients remain insufficiently active (8), particularly when they do not participate in CRP (9,10). Hence, it is important to understand factors related to being physically active in order to develop effective interventions to elicit regular PA.
Extensive research has revealed demographic, psychosocial, behavioral, and environmental factors were to be associated with participation in regular PA in healthy, non-diseased populations (11). However, few studies have examined correlates of PA in cardiac patients, and fewer studies have used objective measures of PA (i.e., accelerometer) in cardiac patients. The purpose of this study was therefore to determine correlates of objectively-measured PA in cardiac patients.
Methods
Participants and settings
Sixty-five (74% male, 95% white, age 58.6±10.6 years) post phase II cardiac patients who were clinically stable and eligible, but not enrolled in maintenance CRP took part in this study. Written informed consent was completed by all patients, and this study was approved by the Institutional Review Boards at Ball State University and Indiana University Health-Ball Memorial Hospital. Patients with any conditions (e.g., heart failure, COPD, orthopedic limitation) that limit habitual PA were excluded from participation. Patient’s participation in PA (min/day) was measured by ActiGraph GT3X accelerometers for 7 consecutive days in order to achieve sufficient reliability (12). The accelerometers were initialized to collect activity counts in 60-second intervals). The amount of time spent in total PA (light-to-vigorous PA) and moderate-to-vigorous PA (MVPA) was assessed using previously validated accelerometer cut points in adults (total PA ≥100, MVPA ≥1,952 counts/min (13,14). All potential correlates were measured via self-reported questionnaire or clinical examinations. Each participant completed a questionnaire on health-related psychosocial and behavioral factors, and underwent a thorough clinical examination that included anthropometry measurement, dual-energy X-ray absorptiometry (DXA) scan, functional capacity test (6-minute walk test), blood pressure measurement, and fasting blood chemistry analyses. A total of 25 potential correlates of PA were measured across four domains: (I) socio-demographic; (II) clinical; (III) psychosocial; and (IV) behavioral. The names and definitions of 25 potential correlates are presented in Table 1.

Full table
Statistical analyses
Pearson correlation coefficients between all potential correlates and PA were estimated, and then only correlates with P values of <15 were selected for the final model building process. Backward elimination model selection procedures were performed to examine associations of potential determinants with total PA and MVPA using SAS (Version 9.3, NC, USA). Statistical significance was set at α =05.
Results
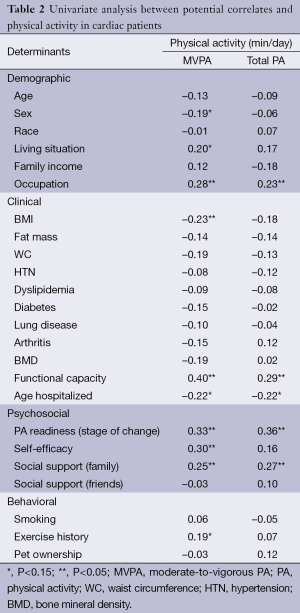
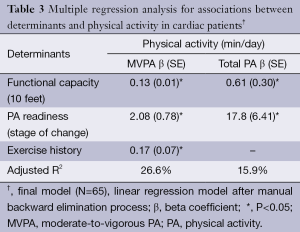
Descriptive statistics of potential correlates and participants’ clinical characteristics including PA levels are presented in Table 1. On average, cardiac patients spent 8.4±8.1 and 153.8±62.8 min/day in MVPA and total PA, respectively. The univariate analyses showed that ten and five factors across four domains were significantly correlated with MVPA and total PA, respectively (Table 2). In the final model (Table 3), functional capacity, PA readiness, and exercise history were directly associated with MVPA (adjusted R2 =27%). Functional capacity and PA readiness were also directly associated with total PA in the final model (adjusted R2 =16%).
Full table
Full table
Discussion
To the best of our knowledge, this was the first study including objective measures of PA and factors across multiple domains to determine correlates of PA in cardiac patients. A key finding of this study was that three factors across clinical (functional capacity), psychosocial (PA readiness), and behavioral domains (exercise history for MVPA only) were identified as positive correlates of cardiac patients’ participation in PA. We also found that most (98%) of cardiac patients in this study were insufficiently active (MVPA <150 min/week). As the cardiac rehabilitation is a multicomponent intervention, these findings are particularly important to clinicians and researchers because they suggest that PA inventions for cardiac patients or CRP should be developed with consideration of factors across multiple.
In a recent review, past participation in exercise was one of the most consistent correlates of PA in cardiac patients (15). In the current study we observed a direct association between exercise history and patients’ current levels of MVPA. Although past behavior is not modifiable, this finding provides an important consideration for future interventions, that previously inactive cardiac patients are in a great need of PA interventions. In addition, we found that functional capacity was a consistent positive correlate for both MVPA and total PA. Recent studies also showed that functional capacity was directly associated with PA in cardiac patients (15,16), implying that interventions to promote PA should include components specifically aiming to increase functional capacity in this patient population.
PA readiness, also known as Stages of Change, was positively associated with both MVPA and total PA. In the context of PA, Stages of Change postulates that individuals progress through different stages of readiness as they change levels of PA (17). Evidence showed that PA readiness was positively associated with PA participation in cardiac patients (18,19). Consequently, these findings suggest that assessing and incorporating PA readiness is beneficial to maximize the effectiveness of PA interventions or CRP.
Social support by family and friends has been found as a consistent psychosocial correlate in healthy populations (11); however, it was not a significant correlate in this study. Although previous studies have reported significant associations between social supports and PA in cardiac patients (20), null associations were not uncommon (16), thus the influence of social support on cardiac patient’s PA remain inconclusive (15).
All three of the correlates of PA, exercise history, functional capacity, and PA readiness, found in the current study are consistent with previous observations in the literature (15,16,18,19). Thus, consideration of these factors is important for CR Program Directors and clinicians when working with cardiac patients in a PA intervention. Cardiac patients without a history of exercise, and/or those with a lower functional capacity, and/or those in the pre-contemplation or contemplation stages of change may have a more difficult time achieving success in the PA intervention program. These patients will likely need more attention and assistance in the form of education and counseling to change their PA behavior. Additionally, interventions that provide a more individualized approach to increasing PA (e.g., increasing daily steps by 10% of their current level each week) may be more appropriate for patients with these characteristics. Patients who do comply with the PA intervention should obtain functional capacity improvements, which then could lead to longer-term compliance.
Strengths of this study include comprehensive measures of potential correlates and objectively-measured PA. Cross-sectional design and lack of information on environmental factors represent limitations of the current study, therefore prospective studies including larger samples and more potential correlates are warranted to better understand determinants of PA in cardiac patients.
In summary, functional capacity, PA readiness, and exercise history were shown to be important factors influencing cardiac patients’ PA. Considering the low levels of PA in cardiac patients, interventions or CRP should include correlates identified in this study as their key components to promote PA in cardiac patients.
Acknowledgements
We thank the cardiopulmonary rehabilitation team at IU Health - Ball Memorial Hospital and research staff at Ball State University’s Human Performance Laboratory for their assistance for this study. We also thank American Heart Association for the grant support (AHA Midwest Affiliate Grant-in-Aid) for this study.
Authors’ contributions: WB has contributed to the design, data analysis, and manuscript preparation. CO, KR, SS, and LK contributed to the initiation the study and the acquisition of the data, interpretation of the data, and assistance with the manuscript preparation.
Disclosure: The authors declare no conflict of interest.
References
- World Health Organization. Causes of death 2008. World Health Organization. Geneva: Department of Health Statistics and Informatics; 2011.
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 2013;127:e6-e245. [PubMed]
- Austin J, Williams WR, Ross L, et al. Five-year follow-up findings from a randomized controlled trial of cardiac rehabilitation for heart failure. Eur J Cardiovasc Prev Rehabil 2008;15:162-7. [PubMed]
- Mampuya WM. Cardiac rehabilitation past, present and future: an overview. Cardiovasc Diagn Ther 2012;2:38-49. [PubMed]
- Hamer M, Stamatakis E. Physical activity and mortality in men and women with diagnosed cardiovascular disease. Eur J Cardiovasc Prev Rehabil 2009;16:156-60. [PubMed]
- Swift DL, Lavie CJ, Johannsen NM, et al. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J 2013;77:281-92. [PubMed]
- Moholdt T, Wisløff U, Nilsen TI, et al. Physical activity and mortality in men and women with coronary heart disease: a prospective population-based cohort study in Norway (the HUNT study). Eur J Cardiovasc Prev Rehabil 2008;15:639-45. [PubMed]
- Stevenson TG, Riggin K, Nagelkirk PR, et al. Physical activity habits of cardiac patients participating in an early outpatient rehabilitation program. J Cardiopulm Rehabil Prev 2009;29:299-303. [PubMed]
- Guiraud T, Granger R, Gremeaux V, et al. Accelerometer as a tool to assess sedentarity and adherence to physical activity recommendations after cardiac rehabilitation program. Ann Phys Rehabil Med 2012;55:312-21. [PubMed]
- Kaminsky LA, Jones J, Riggin K, et al. A pedometer-based physical activity intervention for patients entering a maintenance cardiac rehabilitation program: a pilot study. Cardiovasc Diagn Ther 2013;3:73-9. [PubMed]
- Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet 2012;380:258-71. [PubMed]
- tthews CE, Ainsworth BE, Thompson RW, et al. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc 2002;34:1376-81.
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc 1998;30:777-81. [PubMed]
- Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol 2008;167:875-81. [PubMed]
- Petter M, Blanchard C, Kemp KA, et al. Correlates of exercise among coronary heart disease patients: review, implications and future directions. Eur J Cardiovasc Prev Rehabil 2009;16:515-26. [PubMed]
- Leung YW, Ceccato N, Stewart DE, et al. A prospective examination of patterns and correlates of exercise maintenance in coronary artery disease patients. J Behav Med 2007;30:411-21. [PubMed]
- Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol 1994;13:39-46. [PubMed]
- Rejeski WJ, Tian L, Liao Y, et al. Social cognitive constructs and the promotion of physical activity in patients with peripheral artery disease. J Cardiopulm Rehabil Prev 2008;28:65-72. [PubMed]
- Schwarzer R, Luszczynska A, Ziegelmann JP, et al. Social-cognitive predictors of physical exercise adherence: three longitudinal studies in rehabilitation. Health Psychol 2008;27:S54-63. [PubMed]
- Moore SM, Dolansky MA, Ruland CM, et al. Predictors of women’s exercise maintenance after cardiac rehabilitation. J Cardiopulm Rehabil 2003;23:40-9. [PubMed]


